Foot and Ankle Procedures
What is VNUS Closure - Radio Frequency Ablation
The VNUS Closure procedure is offered for treating larger varicose veins. The Closure procedure is performed on an outpatient basis by using radiofrequency (RF) energy applied to the inside vein walls of the damaged vessel. This same-day out patient minimal invasive procedure is an alternative treatment option to traditional vein stripping surgery.
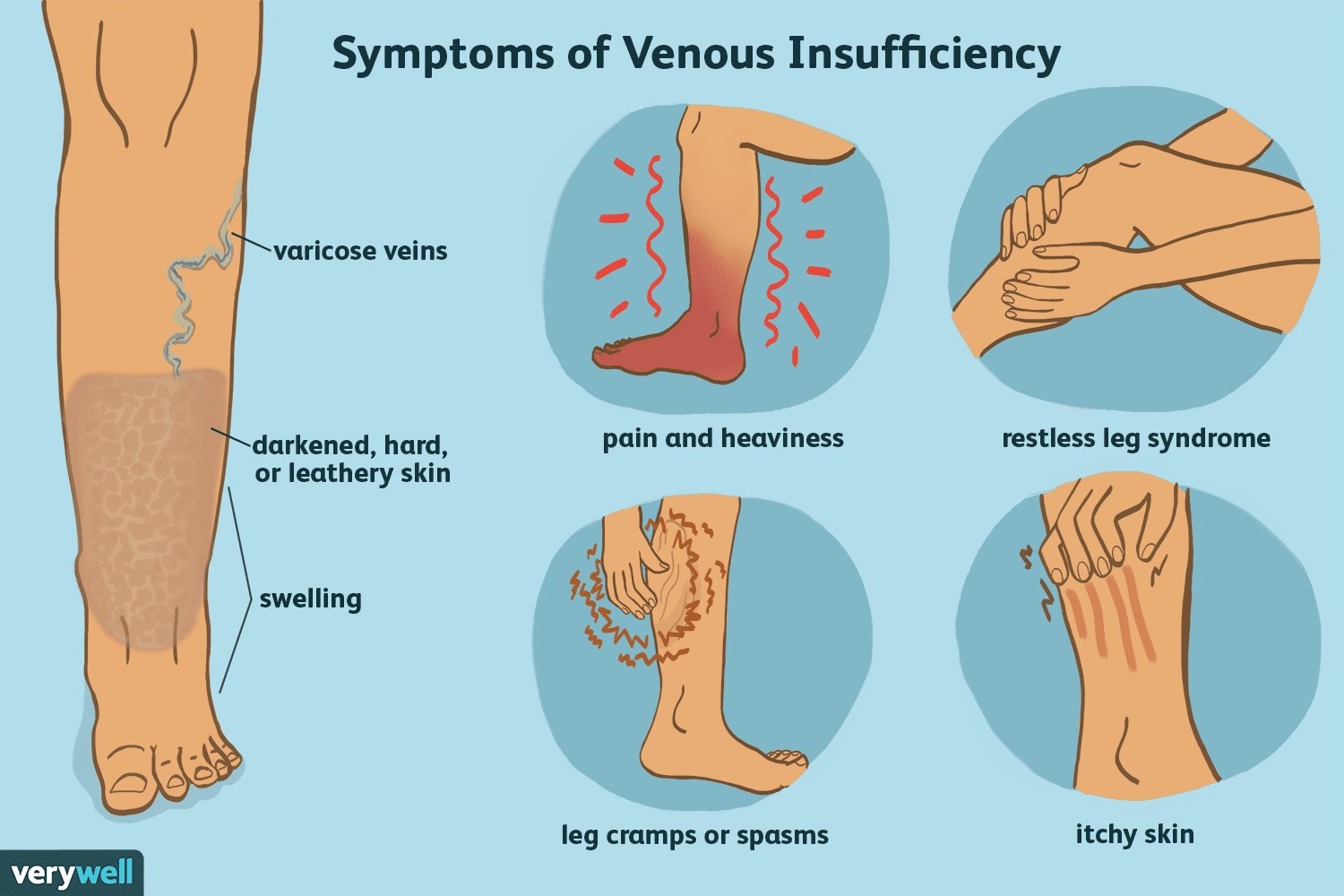
RFA is a treatment for:
venous reflux, also called chronic venous insufficiency, the root cause of varicose veins and achy, tired legs.
A needle size thin catheter is placed in the diseased vein without incisions. The catheter then delivers radiofrequency (RF) energy which causes the diseased vein walls to shrink and close.
Once the diseased vein is closed, blood is re-routed to healthy veins. The circulation actually improves after the vein closure! The procedure takes about 20 minutes and is a minimal invasive procedure. There is virtually no postoperative discomfort.
RECOVERY:
Patients who undergo the Closure procedure often resume normal activities quickly with excellent cosmetic and therapeutic results. Following the procedure, the leg is wrapped in an Ace bandage for 24 hours. Patients are encouraged to walk, which help improve circulation. Patients who undergo the Closure procedure can resume normal activity the same day. Full activity including strenuous exercise can resume after 7 days.
Most people notice an improvement in their symptoms within several days of having the procedure. Studies have shown that the Closure procedure has a 95% long term success rate.
Is RFA covered by insurance?
The procedure is approved by the FDA and is covered by medical insurance plans and Medicare.
Even though bunions are a common foot deformity, there are misconceptions about them. Many people may unnecessarily suffer the pain of bunions for years before seeking treatment.
What is a Bunionectomy
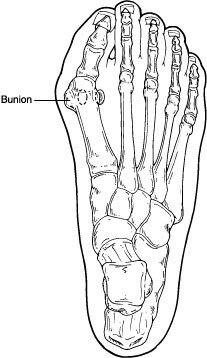 A bunion is often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. The big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment—producing the bunion’s bump.
A bunion is often described as a bump on the side of the big toe. But a bunion is more than that. The visible bump actually reflects changes in the bony framework of the front part of the foot. The big toe leans toward the second toe, rather than pointing straight ahead. This throws the bones out of alignment—producing the bunion’s bump.
Bunions are a progressive disorder. They begin with a leaning of the big toe, gradually changing the angle of the bones over the years and slowly producing the characteristic bump, which becomes increasingly prominent. Symptoms usually appear at later stages, although some people never have symptoms.
Causes
Bunions are most often caused by an inherited faulty mechanical structure of the foot. It is not the bunion itself that is inherited but certain foot types that make a person prone to developing a bunion.
Although wearing shoes that crowd the toes will not actually cause bunions, it sometimes makes the deformity get progressively worse. Symptoms may therefore appear sooner.
Symptoms
Symptoms, which occur at the site of the bunion, may include:
- Pain or soreness
- Inflammation and redness
- A burning sensation
- Possible numbness
Because bunions are progressive, they do not go away and will usually get worse over time. But not all cases are alike—some bunions progress more rapidly than others. Once your surgeon has evaluated your bunion, a treatment plan can be developed that is suited to your needs.
When Is Surgery Needed?
If nonsurgical treatments fail to relieve bunion pain and when the pain of a bunion interferes with daily activities, it is time to discuss surgical options with a foot and ankle surgeon. Together you can decide if surgery is best for you.
A variety of surgical procedures is available to treat bunions. The procedures are designed to remove the bump of bone, correct the changes in the bony structure of the foot and correct soft tissue changes that may also have occurred. The goal of surgery is the reduction of pain and deformity.
In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity based on the x-ray findings, your age, your activity level and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
TO FIX: PAINFUL BUNION DEFORMITY, PAINFUL BONE GROWTH TO THE FOOT
What Is Hammertoe?
Hammertoe is a contracture (bending) deformity of one or both joints of the second, third, fourth or fifth (little) toes. This abnormal bending can put pressure on the toe when wearing shoes, causing problems to develop.
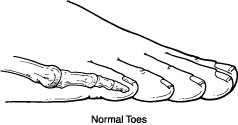
Hammertoes usually start out as mild deformities and get progressively worse over time. In the earlier stages, hammertoes are flexible and the symptoms can often be managed with noninvasive measures. But if left untreated, hammertoes can become more rigid and will not respond to nonsurgical treatment.

Because of the progressive nature of hammertoes, they should receive early attention. Hammertoes never get better without some kind of intervention.
Causes
The most common cause of hammertoe is a muscle/tendon imbalance. This imbalance, which leads to a bending of the toe, results from mechanical (structural) or neurological changes in the foot that occur over time in some people.
Hammertoes may be aggravated by shoes that do not fit properly. A hammertoe may result if a toe is too long and is forced into a cramped position when a tight shoe is worn. Occasionally, hammertoe is the result of an earlier trauma to the toe. In some people, hammertoes are inherited.
Symptoms
Common symptoms of hammertoes include:
- Pain or irritation of the affected toe when wearing shoes.
- Corns and calluses (a buildup of skin) on the toe, between two toes or on the ball of the foot. Corns are caused by constant friction against the shoe. They may be soft or hard, depending on their location.
- Inflammation, redness or a burning sensation
- Contracture of the toe
- In more severe cases of hammertoe, open sores may form
Diagnosis
Although hammertoes are readily apparent, to arrive at a diagnosis, the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. During the physical examination, the doctor may attempt to reproduce your symptoms by manipulating your foot and will study the contractures of the toes. In addition, the foot and ankle surgeon may take x-rays to determine the degree of the deformities and assess any changes that may have occurred.
Hammertoes are progressive—they do not go away by themselves and usually they will get worse over time. However, not all cases are alike—some hammertoes progress more rapidly than others. Once your foot and ankle surgeon has evaluated your hammertoes, a treatment plan can be developed that is suited to your needs.
When Is Surgery Needed?
In some cases, usually when the hammertoe has become more rigid and painful or when an open sore has developed, surgery is needed. Often, patients with hammertoe have bunions or other foot deformities corrected at the same time. In selecting the procedure or combination of procedures for your particular case, the foot and ankle surgeon will take into consideration the extent of your deformity, the number of toes involved, your age, your activity level and other factors. The length of the recovery period will vary, depending on the procedure or procedures performed.
What Is a Ganglion Cyst?
A ganglion cyst is a sac filled with a jellylike fluid that originates from a tendon sheath or joint capsule. The word “ganglion” means knot and is used to describe the knot-like mass or lump that forms below the surface of the skin.
Ganglion cysts are among the most common benign soft-tissue masses. Although they most often occur on the wrist, they also frequently develop on the foot—usually on the top, but elsewhere as well. Ganglion cysts vary in size, may get smaller and larger and may even disappear completely, only to return later.
Causes
Although the exact cause of ganglion cysts is unknown, they may arise from trauma—whether a single event or repetitive microtrauma.
Symptoms
A ganglion cyst is associated with one or more of the following symptoms:
- A noticeable lump—often this is the only symptom experienced
- Tingling or burning, if the cyst is touching a nerve
- Dull pain or ache, which may indicate the cyst is pressing against a tendon or joint
- Difficulty wearing shoes due to irritation between the lump and the shoe
Diagnosis
To diagnose a ganglion cyst, the foot and ankle surgeon will perform a thorough examination of the foot. The lump will be visually apparent, and, when pressed in a certain way, it should move freely underneath the skin. Sometimes the surgeon will shine a light through the cyst or remove a small amount of fluid from the cyst for evaluation. Your doctor may take an x-ray, and in some cases, additional imaging studies may be ordered.
When Is Surgery Needed?
When other treatment options fail or are not appropriate, the cyst may need to be surgically removed. While the recurrence rate associated with surgery is much lower than that experienced with aspiration and injection therapy, there are nevertheless cases in which the ganglion cyst returns. Surgery is highly recommended for recurrent ganglion cyst.
What Is a Soft-Tissue Biopsy?
A soft-tissue biopsy is the removal and microscopic examination of a small sample of soft tissue for diagnostic purposes. Soft tissue includes the skin, fat, muscle and tendons that surround, connect or support other tissues or organs. Soft-tissue biopsies require little time or involvement from the patient. They enable the foot and ankle surgeon to reach an accurate diagnosis and to determine the best treatment for the specific condition.
Conditions Identified by Soft-Tissue Biopsies
- Freckles (macules)
- Benign pigmented, or colored, spots (moles or nevus)
- Fungal or bacterial infections
- Rashes (such as eczema or dermatitis)
- Lesions related to a disease affecting the entire body (such as diabetes)
- Nodular conditions (such as a ganglion cyst, lipoma or fibroma)
- Toenail conditions (onychomycosis, psoriasis)
- Wart-like growths on the skin (benign keratoses)
- Premalignant conditions (actinic and seborrheic keratoses)
What Does the Biopsy Involve?
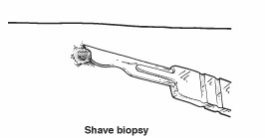
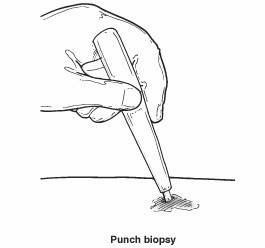
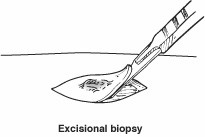
A biopsy involves removal of a small piece of tissue and takes just a few minutes. The procedure performed will depend on the tissue to be sampled. After numbing the area, the surgeon performs one of the following:
Shave biopsy. A thin piece of tissue is shaved off.
Punch biopsy. A small, round instrument removes a tiny core of tissue. Stitches may be needed.
Incisional or excisional biopsy. A piece, or the entire lesion, is removed. Stitches are often needed.
Once the sample is obtained, the surgeon sends it to a clinical laboratory so that the condition can be identified. The specimen will be examined by a pathologist who specializes in evaluating soft-tissue biopsies.
After the Biopsy
Patients should follow the instructions provided by the surgeon for care of the biopsy site. If the area has stitches, an appointment will be scheduled for their removal. It usually takes several days for the lab results to arrive at the surgeon’s office. If the patient has not heard about the results after 10 days, the surgeon’s office should be contacted. Biopsy results, as well as additional treatment that may be required, will then be discussed.
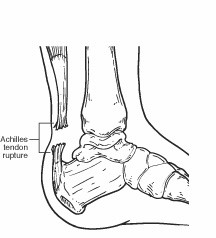
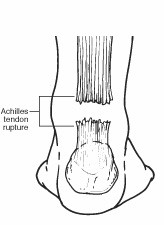
What Is the Achilles Tendon?
A tendon is a band of tissue that connects a muscle to a bone. The Achilles tendon runs down the back of the lower leg and connects the calf muscle to the heel bone. Also called the heel cord, the Achilles tendon facilitates walking by helping to raise the heel off the ground.
What Is an Achilles Tendon Rupture?
An Achilles tendon rupture is a complete or partial tear that occurs when the tendon is stretched beyond its capacity. Forceful jumping or pivoting, or sudden accelerations of running, can overstretch the tendon and cause a tear. An injury to the tendon can also result from falling or tripping.
Achilles tendon ruptures are most often seen in "weekend warriors"—typically, middle-aged people participating in sports in their spare time. Less commonly, illness or medications, such as steroids or certain antibiotics, may weaken the tendon and contribute to ruptures.
Signs & Symptoms
A person with a ruptured Achilles tendon may experience one or more of the following:
- Sudden pain (which feels like a kick or a stab) in the back of the ankle or calf—often subsiding into a dull ache
- A popping or snapping sensation
- Swelling on the back of the leg between the heel and the calf
- Difficulty walking (especially upstairs or uphill) and difficulty rising up on the toe
These symptoms require prompt medical attention to prevent further damage. Until the patient is able to see a doctor, the RICE method should be used. This involves:
- Rest. Stay off the injured foot and ankle, since walking can cause pain or further damage.
- Ice. Apply a bag of ice covered with a thin towel to reduce swelling and pain. Do not put ice directly against the skin.
- Compression. Wrap the foot and ankle in an elastic bandage to prevent further swelling.
- Elevation. Keep the leg elevated to reduce the swelling. It should be even with or slightly above heart level.
Diagnosis
In diagnosing an Achilles tendon rupture, the foot and ankle surgeon will ask questions about how and when the injury occurred and whether the patient has previously injured the tendon or experienced similar symptoms. The surgeon will examine the foot and ankle, feeling for a defect in the tendon that suggests a tear. Range of motion and muscle strength will be evaluated and compared to the uninjured foot and ankle. If the Achilles tendon is ruptured, the patient will have less strength in pushing down (as on a gas pedal) and will have difficulty rising on the toes.
The diagnosis of an Achilles tendon rupture is typically straightforward and can be made through this type of examination. In some cases, however, the surgeon may order an MRI or other advanced imaging tests.
Treatment
Treatment options for an Achilles tendon rupture include surgical and nonsurgical approaches. The decision of whether to proceed with surgery or nonsurgical treatment is based on the severity of the rupture and the patient’s health status and activity level.
Surgery
Surgery offers important potential benefits. Besides decreasing the likelihood of rerupturing the Achilles tendon, surgery often increases the patient’s push-off strength and improves muscle function and movement of the ankle.
Various surgical techniques are available to repair the rupture. The surgeon will select the procedure best suited to the patient.
Following surgery, the foot and ankle are initially immobilized in a cast or walking boot. The surgeon will determine when the patient can begin weightbearing.
Complications such as incision-healing difficulties, rerupture of the tendon or nerve pain can arise after surgery.
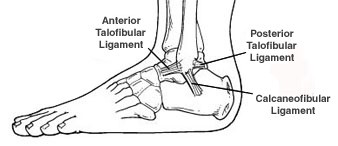
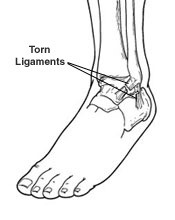
What Is an Ankle Sprain?
An ankle sprain is an injury to one or more ligaments in the ankle, usually on the outside of the ankle. Ligaments are bands of tissue—like rubber bands—that connect one bone to another and bind the joints together. In the ankle joint, ligaments provide stability by limiting side-to-side movement.
Some ankle sprains are much worse than others. The severity of an ankle sprain depends on whether the ligament is stretched, partially torn or completely torn, as well as on the number of ligaments involved. Ankle sprains are not the same as strains, which affect muscles rather than ligaments.
Causes
Sprained ankles often result from a fall, a sudden twist or a blow that forces the ankle joint out of its normal position. Ankle sprains commonly occur while participating in sports, wearing inappropriate shoes or walking or running on an uneven surface.
Sometimes ankle sprains occur because a person is born with weak ankles. Previous ankle or foot injuries can also weaken the ankle and lead to sprains.
Symptoms
The symptoms of ankle sprains may include:
- Pain or soreness
- Swelling
- Bruising
- Difficulty walking
- Stiffness in the joint
Ankle fractures are common injuries most often caused by the ankle rolling inward or outward. Many people mistake an ankle fracture for an ankle sprain, but they are quite different and therefore require an accurate and early diagnosis. They sometimes occur simultaneously.
Why Prompt Medical Attention Is Needed
There are four key reasons why an ankle sprain should be promptly evaluated and treated by a foot and ankle surgeon:
- An untreated ankle sprain may lead to chronic ankle instability, a condition marked by persistent discomfort and a giving way of the ankle. Weakness in the leg may also develop.
- A more severe ankle injury may have occurred along with the sprain. This might include a serious bone fracture that, if left untreated, could lead to troubling complications.
- An ankle sprain may be accompanied by a foot injury that causes discomfort but has gone unnoticed thus far.
- Rehabilitation of a sprained ankle needs to begin right away. If rehabilitation is delayed, the injury may be less likely to heal properly.
Diagnosis
In evaluating your injury, the foot and ankle surgeon will obtain a thorough history of your symptoms and examine your foot. X-rays or other advanced imaging studies may be ordered to help determine the severity of the injury.
When Is Surgery Needed?
In more severe cases, surgery may be required to adequately treat an ankle sprain. Surgery often involves repairing the damaged ligament or ligaments. The foot and ankle surgeon will select the surgical procedure best suited for your case based on the type and severity of your injury as well as your activity level.
After surgery, rehabilitation is extremely important. Completing your rehabilitation program is crucial to a successful outcome. Be sure to continue to see your foot and ankle surgeon during this period to ensure that your ankle heals properly and function is restored.
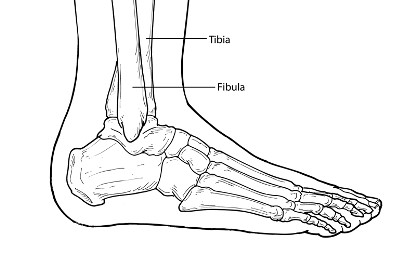
What Is an Ankle Fracture?
A fracture is a partial or complete break in a bone. Fractures in the ankle can range from the less serious avulsion injuries (small pieces of bone that have been pulled off) to severe shattering-type breaks of the tibia, fibula or both.
Ankle fractures are common injuries most often caused by the ankle rolling inward or outward. Many people mistake an ankle fracture for an ankle sprain, but they are quite different and therefore require an accurate and early diagnosis. They sometimes occur simultaneously.
Symptoms
An ankle fracture is accompanied by one or all of these symptoms:
- Pain at the site of the fracture, which in some cases can extend from the foot to the knee.
- Significant swelling, which may occur along the length of the leg or may be more localized.
- Blisters may occur over the fracture site. These should be promptly treated by a foot and ankle surgeon.
- Bruising that develops soon after the injury.
- Inability to walk; however, it is possible to walk with less severe breaks, so never rely on walking as a test of whether or not a bone has been fractured.
- Change in the appearance of the ankle—it will look different from the other ankle.
- Bone protruding through the skin—a sign that immediate care is needed. Fractures that pierce the skin require immediate attention because they can lead to severe infection and prolonged recovery.
Diagnosis
Following an ankle injury, it is important to have the ankle evaluated by a foot and ankle surgeon for proper diagnosis and treatment. If you are unable to do so right away, go to the emergency room and then follow up with a foot and ankle surgeon as soon as possible for a more thorough assessment.
The affected limb will be examined by the foot and ankle surgeon who will touch specific areas to evaluate the
When Is Surgery Needed?
For some ankle fractures, surgery is needed to repair the fracture and other soft tissue-related injuries, if present. The foot and ankle surgeon will select the procedure that is appropriate for your injury. Surgical intervention may involve from staples to screws and plates.
Follow-Up Care
It is important to follow your surgeon’s instructions after treatment. Failure to do so can lead to infection, deformity, arthritis and chronic pain.
What Is Equinus?
Equinus is a condition in which the upward bending motion of the ankle joint is limited. Someone with equinus lacks the flexibility to bring the top of the foot toward the front of the leg. Equinus can occur in one or both feet. When it involves both feet, the limitation of motion is sometimes worse in one foot than in the other.
People with equinus develop ways to compensate for their limited ankle motion, and this often leads to other foot, leg or back problems. The most common methods of compensation are flattening of the arch or picking up the heel early when walking, placing increased pressure on the ball of the foot. Other patients compensate by toe walking, while a smaller number take steps by bending abnormally at the hip or knee.
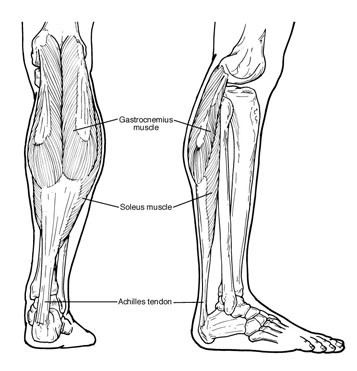
Causes
There are several possible causes for the limited range of ankle motion. Often, it is due to tightness in the Achilles tendon or calf muscles (the soleus muscle and/or gastrocnemius muscle). In some patients, this tightness is congenital (present at birth), and sometimes it is an inherited trait. Other patients acquire the tightness from being in a cast, being on crutches or frequently wearing high-heeled shoes. In addition, diabetes can affect the fibers of the Achilles tendon and cause tightness. Sometimes equinus is related to a bone blocking the ankle motion. For example, a fragment of a broken bone following an ankle injury, or bone block, can get in the way and restrict motion. Equinus may also result from one leg being shorter than the other. Less often, equinus is caused by spasms in the calf muscle. These spasms may be signs of an underlying neurologic disorder.
Foot Problems Related to Equinus
Depending on how a patient compensates for the inability to bend properly at the ankle, a variety of foot conditions can develop, including:
- Plantar fasciitis (arch/heel pain)
- Calf cramping
- Tendonitis (inflammation in the Achilles tendon)
- Metatarsalgia (pain and/or callusing on the ball of the foot)
- Flatfoot
- Arthritis of the midfoot (middle area of the foot)
- Pressure sores on the ball of the foot or the arch
- Bunions and hammertoes
- Ankle pain
- Shin splints
Diagnosis
Most patients with equinus are unaware they have this condition when they first visit the doctor. Instead, they come to the doctor seeking relief for foot problems associated with equinus.
To diagnose equinus, the foot and ankle surgeon will evaluate the ankle's range of motion when the knee is flexed (bent) as well as extended (straightened). This enables the surgeon to identify whether the tendon or muscle is tight and to assess whether bone is interfering with ankle motion. X-rays may also be ordered. In some cases, the foot and ankle surgeon may refer the patient for neurologic evaluation.
When Is Surgery Needed?
Surgery may be needed to correct the cause of equinus if it is related to a tight achilles tendon preventing full function of the lower extremity or a bone blocking the ankle motion. The foot and ankle surgeon will determine the type of procedure that is best suited to the individual patient.
What Is PTTD?
The posterior tibial tendon serves as one of the major supporting structures of the foot, helping it to function while walking. Posterior tibial tendon dysfunction (PTTD) is a condition caused by changes in the tendon, impairing its ability to support the arch. This results in flattening of the foot.
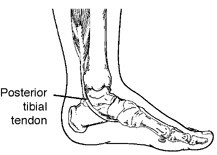
PTTD is often called adult acquired flatfoot because it is the most common type of flatfoot developed during adulthood. Although this condition typically occurs in only one foot, some people may develop it in both feet. PTTD is usually progressive, which means it will keep getting worse, especially if it is not treated early.
Causes
Overuse of the posterior tibial tendon is often the cause of PTTD. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking or climbing stairs.

Symptoms
The symptoms of PTTD may include pain, swelling, a flattening of the arch and an inward rolling of the ankle. As the condition progresses, the symptoms will change.
For example, when PTTD initially develops, there is pain on the inside of the foot and ankle (along the course of the tendon). In addition, the area may be red, warm and swollen.
Later, as the arch begins to flatten, there may still be pain on the inside of the foot and ankle. But at this point, the foot and toes begin to turn outward and the ankle rolls inward.
As PTTD becomes more advanced, the arch flattens even more and the pain often shifts to the outside of the foot, below the ankle. The tendon has deteriorated considerably, and arthritis often develops in the foot. In more severe cases, arthritis may also develop in the ankle.
When Is Surgery Needed?
For some advanced cases, surgery may be the only option. Your foot and ankle surgeon will determine the best approach for you after having reviewed your MRI and and CT report. Surgical procedure for PTTD repair can often result in a slow recovery. However, once recovered, patients are significantly happier. It is important to review all surgical options with your surgeon.
What Is Chronic Ankle Instability?
Chronic ankle instability is a condition characterized by a recurring giving way of the outer (lateral) side of the ankle. This condition often develops after repeated ankle sprains. Usually, the giving way occurs while walking or doing other activities, but it can also happen when you’re just standing. Many athletes, as well as others, suffer from chronic ankle instability.

People with chronic ankle instability often complain of:
- A repeated turning of the ankle, especially on uneven surfaces or when participating in sports
- Persistent (chronic) discomfort and swelling
- Pain or tenderness
- The ankle feeling wobbly or unstable
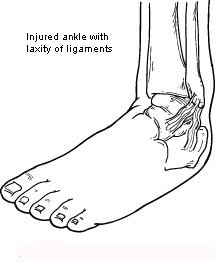
Causes
Chronic ankle instability usually develops following an ankle sprain that has not adequately healed or was not rehabilitated completely. When you sprain your ankle, the connective tissues (ligaments) are stretched or torn. The ability to balance is often affected. Proper rehabilitation is needed to strengthen the muscles around the ankle and retrain the tissues within the ankle that affect balance. Failure to do so may result in repeated ankle sprains.
Repeated ankle sprains often cause—and perpetuate—chronic ankle instability. Each subsequent sprain leads to further weakening (or stretching) of the ligaments, resulting in greater instability and the likelihood of developing additional problems in the ankle.
Diagnosis
In evaluating and diagnosing your condition, the foot and ankle surgeon will ask you about any previous ankle injuries and instability. Then s/he will examine your ankle to check for tender areas, signs of swelling and instability of your ankle as shown in the illustration. X-rays or other imaging studies may be helpful in further evaluating the ankle.
When Is Surgery Needed?
In some cases, the foot and ankle surgeon will recommend surgery based on the degree of instability or lack of response to nonsurgical approaches. Surgery usually involves repair or reconstruction of the damaged ligament(s). The surgeon will select the surgical procedure best suited for your case based on the severity of the instability and your activity level. The length of the recovery period will vary, depending on the procedure or procedures performed.
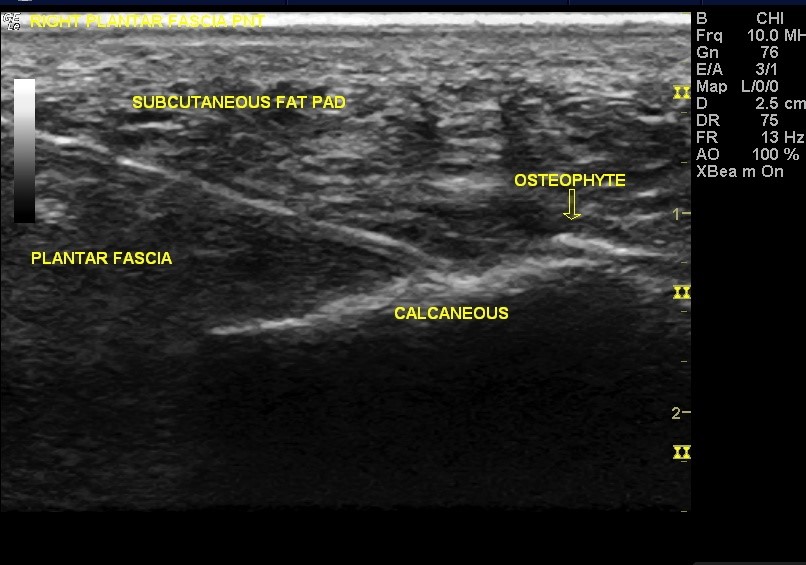
Heel pain is most often caused by plantar fasciitis, a condition that is sometimes also called heel spur syndrome when a spur is present. Heel pain may also be due to other causes, such as a stress fracture, tendonitis, arthritis, nerve irritation or, rarely, a cyst.
Because there are several potential causes, it is important to have heel pain properly diagnosed. A foot and ankle surgeon is able to distinguish between all the possibilities and to determine the underlying source of your heel pain.
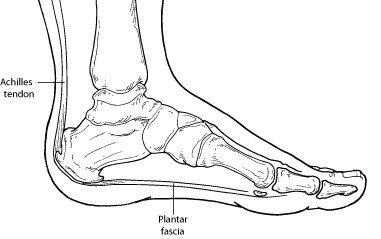
What Is Plantar Fasciitis?
Plantar fasciitis is an inflammation of the band of tissue (the plantar fascia) that extends from the heel to the toes. In this condition, the fascia first becomes irritated and then inflamed, resulting in heel pain.
Causes
The most common cause of plantar fasciitis relates to faulty structure of the foot. For example, people who have problems with their arches, either overly flat feet or high-arched feet, are more prone to developing plantar fasciitis.
Wearing nonsupportive footwear on hard, flat surfaces puts abnormal strain on the plantar fascia and can also lead to plantar fasciitis. This is particularly evident when one’s job requires long hours on the feet. Obesity and overuse may also contribute to plantar fasciitis.
Symptoms
The symptoms of plantar fasciitis are:
- Pain on the bottom of the heel
- Pain in the arch of the foot
- Pain that is usually worse upon arising
- Pain that increases over a period of months
- Swelling on the bottom of the heel
People with plantar fasciitis often describe the pain as worse when they get up in the morning or after they have been sitting for long periods of time. After a few minutes of walking, the pain decreases because walking stretches the fascia. For some people, the pain subsides but returns after spending long periods of time on their feet.
Diagnosis
To arrive at a diagnosis, the foot and ankle surgeon will obtain your medical history and examine your foot. Throughout this process, the surgeon rules out all possible causes for your heel pain other than plantar fasciitis.
In addition, diagnostic imaging studies, such as x-rays or other imaging modalities, may be used to distinguish the different types of heel pain. Sometimes heel spurs are found in patients with plantar fasciitis, but these are rarely a source of pain. When they are present, the condition may be diagnosed as plantar fasciitis/heel spur syndrome.
When Is Surgery Needed?
Patients may require surgery if the plantar fasciitis has become chronic in nature or if there is a tear detected on MRI.. If, after several months of nonsurgical treatment, you continue to have heel pain, surgery will be considered. Your foot and ankle surgeon will discuss the surgical options with you and determine which approach would be most beneficial for you.
Unique Surgical Procedures done by Dr. Goswami.
These procedures are not typically performed by most foot & ankle surgeons.
What Is a Talar Dome Lesion?
The ankle joint is composed of the bottom of the tibia (shin) bone and the top of the talus (ankle) bone. The top of the talus is dome-shaped and is completely covered with cartilage—a tough, rubbery tissue that enables the ankle to move smoothly. A talar dome lesion is an injury to the cartilage and underlying bone of the talus within the ankle joint. It is also called an osteochondral defect (OCD) or osteochondral lesion of the talus (OLT). “Osteo” means bone and “chondral” refers to cartilage.
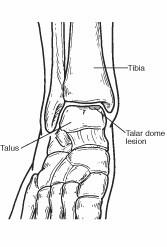
Talar dome lesions are usually caused by an injury, such as an ankle sprain. If the cartilage does not heal properly following the injury, it softens and begins to break off. Sometimes a broken piece of the damaged cartilage and bone will float in the ankle.
Signs & Symptoms
Unless the injury is extensive, it may take months, a year or even longer for symptoms to develop. The signs and symptoms of a talar dome lesion may include:
- Chronic pain deep in the ankle—typically worse when bearing weight on the foot (especially during sports) and less when resting
- An occasional clicking or catching feeling in the ankle when walking
- A sensation of the ankle locking or giving out
- Episodes of swelling of the ankle—occurring when bearing weight and subsiding when at rest
Diagnosis
A talar dome lesion can be difficult to diagnose because the precise site of the pain can be hard to pinpoint. To diagnose this injury, the foot and ankle surgeon will question the patient about recent or previous injury and will examine the foot and ankle, moving the ankle joint to help determine if there is pain, clicking or limited motion within that joint.
Sometimes the surgeon will inject the joint with an anesthetic (pain-relieving medication) to see if the pain goes away for a while, indicating that the pain is coming from inside the joint. X-rays are taken, and often an MRI or other advanced imaging tests are ordered to further evaluate the lesion and extent of the injury.
Operative Treatment
Surgery may involve removal of the loose bone and cartilage fragments within the joint and establishing an environment for healing. A variety of surgical techniques is available to accomplish this. Most surgeons do not attempt to optimize the healing potential upon debridement and repair of the lesion.
My Unique Technique:
Upon removal or debridement of the osteochondritis lesion, we replace the dead defective tissue with either an autograft or allograft tissue. Additional option includes stem cell injection into the ankle joint in association with microfracture to promote cartilaginous growth to the ankle joint. The combination of microfracture with stem cell application provides significant promotion for cartilage replacement and provides the patient a much better surgical outcome as the stem cells are replacing the cartilage of the ankle joint.
The addition of stem cells, allograft or autograft tissue provides the benefit of a more dynamic assessment of the lesion and the severity of lesion instability and assessment of injury to the overlying cartilage. These techniques would also be applied to defects that are larger than 5mm. Most of these operative treatments are performed as an arthroscopic outpatient procedure. Often patients need to undergo a period of non-weight bearing with either cast or brace immobilization to promote healing for approximately 6-8 weeks after surgery.
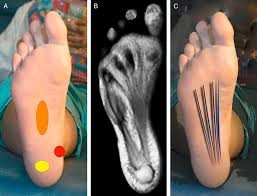
Radiofrequency nerve ablation (RFNA) is a minimally invasive procedure that has been employed to relieve chronic pain associated with plantar fasciitis. Application of radiofrequency energy causes thermal desensitization to the nerve. This dramatically reduces or eliminates the perception of chronic heel pain.
After intradermal injection of a local anesthetic, a radiofrequency cannula is inserted into the heel. Next, the radiofrequency probe is advanced through the cannula and the temperature of the tip is increased to 90°C for 90 seconds.
Next, we inject local anesthetic into the surrounding skin, soft tissue and fascia. With ultrasound guidance, we advance the needle within the damaged fascia. Using a peppering technique, we inject PRP growth factors over the damaged plantar fascial region to allow for an increase in the body’s own inflammatory response. The combination of growth factors harvested from your own blood with increased inflammation jump starts a cascade of soft tissue healing along the chronically damaged ligament.
The procedure can be performed in 10 minutes or less. Following the quick procedure, the patient wears a controlled ankle motion (CAM) walker boot to provide support and decrease stress on the plantar fascia. The boot is worn for one week while weight-bearing as tolerated and then transitions into a stability/motion control running shoe. Within a week to two weeks, patients report returning to normal activity.
WHY DOES RADIOFREQUENCY (RFNA) WORK FOR HEEL PAIN?
Plantar fasciitis involves tearing and inflammation of a ligament (the plantar fascia) which is attached to the heel bone. The plantar fascia sends pain back to the spinal cord and brain via one nerve, the inferior calcaneal nerve. RFNA stops function of this nerve to eliminate heel pain.
What is Plantar fasciitis?
Plantar fasciitis is a common cause of significant heel pain in adults and accounting for approximately 11% to 15% of all foot problems. Multiple treatment modalities are employed for treatment chronic plantar fasciitis including nonsteroidal anti-inflammatory drugs (NSAID), massages, activity modifications, orthoses, local infiltration of steroids and shock wave therapy.
Aggressive surgical techniques have been reported such as open plantar fasciotomy with heel spur resection with often leave patients with prolong recovery time, discomfort and slow healing rate.
The percutaneous plantar fasciotomy procedure, however, is a simple procedure with rare complications.
The ultrasound guided percutaneous plantar fasciotomy allows what was once major surgery to be performed quickly through a small incision. A percutaneous plantar fasciotomy is done through a 1cm incision on the heel involving the damaged ligament.
The foot and toes are positioned to place tension on the involved plantar fascia. Next, using the ultrasound images, the exact position of the damaged plantar fascia is visualized. Once the exact location of the damaged ligament identified, the 1cm incision is made at the bottom of the heel. Under direct ultrasound guidance, the damaged plantar fascia is palpated and identified. Once visualized and identified to the exact location of the damaged ligament, the ligament is carefully released and the incision is closed using one to two stitches.
With the damaged plantar fascia released and an incision of only 1cm, patients can place partial weight on the involved surgical foot and walk home the same day. Recovery time is usually less than 2 weeks.
Injectable human placental tissue allografts and stem cell is a new cutting edge technique in regenerative medicine. This injectable contains collagen, fibronectin, and hyaluronic acid, along with a combination of growth factors, cytokines and anti-inflammatory proteins such as interleukin-1 receptor antagonist.
The human allografts, when injured on an injured tendon or torn ligament, provides a readily available tissue with regenerative properties which harnesses many growth factors, cytokines, proteases, and regulatory inhibitors that can contribute to the process of soft tissue healing. The allografts have shown clinical success in healing poorly vascularized chronic wounds and therefore have promising potential to also promote healing in less vascularize orthopedic tissues like tendon, ligament, and cartilage.
Amniotic membrane-based allografts and stem cells are classified as a naturally derived biomaterial and are currently being used in wound and soft tissue repair applications. It has also been evaluated for repair of tendon and ligament, attenuation of cartilage and arthritic joints. It stimulates cellular activity and provides reparative adult stem cells to the site. The allograft can be used both as a therapy to decrease pain and reduce scar tissue formation.
This minimally invasive procedure is indicated for:
- Chronically damaged Achilles tendonitis as well as tendonitis of the foot and ankle.
- Tendinopathy
- Plantar fasciitis
- Painful foot or ankle ligament injuries from sprain and strains.
- Painful arthritic joints of the foot and ankle; cartilage loss.
- Cartilage and joint space repair
- Ankle instability
- Nerve damage
- Chronic wounds of the foot, ankle and leg
- Diabetic non-healing wounds of the lower extremity
This safe and effective procedure is performed under ultrasound imaging guidance to visualize, the injured soft tissue. Once identified, the injectable human allograft is injected directly into the injured soft tissue. This is an alternative to having an open surgical intervention with much longer recovery time and reduces the chance of post-operative infections. Patients are usually placed on a walking cast or a CAM boot for one to two weeks until the soft tissue is healed.
Current research and clinical cases using amniotic membrane for repairing soft tissues have shown that allografts can have promising results in repairing injured and diseased tissues due to their ability to deliver a natural biomaterial that contains many active biomolecules. There is great for regenerative applications in foot and ankle surgery.
Same Day Surgical Treatments in Altamonte SpingsDavenport DelrayFort Pierce HollywoodMiamiOrlandoPalm Beach GardensCall Us To Make An Appointment
Now Accepting New & Former Laser Spine Institute Patients.
Altamonte Springs
- Address: 499 E. Central Parkway, Suite #130
Altamonte Springs, FL 32701 - Phone: (407) 960-1717
- Fax: (407) 834-2500
Hollywood
- Address: 3500 Tyler Street Hollywood, FL 33021
- Phone: (954) 987-2047
- Fax: (954) 987-2048
Davenport
- Address: 2310 North Blvd, Davenport, FL 33837
- Phone: (407) 960-1717
- Fax: (407) 834-2500
Miami
- Address: 11401 SW 40th St.
Suite # 120
Miami, FL 33165 - Phone: (954) 987-2047
- Fax: (954) 987-2048
Delray
- Address: 15300 Jog Rd,
Suite # 107-108
Delray Beach, FL 33446 - Phone: (561) 630-1611
- Fax: (800) 648-9071
Orlando
- Address: 6150 Metrowest Blvd. Suite #102
Orlando, FL 32835 - Phone: (407) 960-1717
- Fax: (407) 834-2500
Fort Pierce
- Address: 2215 Nebraska Ave
Suite 1C
Fort Pierce, FL 34950 - Phone: (772) 466-0088
- Fax: (772) 460-8555
Palm Beach Gardens
- Address: 3355 Burns Road . Suite 304,
PBG, FL 33410 - Phone: (561) 630-1611
- Fax: (561) 630-1613
Altamonte Springs
- Address: 499 E. Central Parkway,
Suite #130
Altamonte Springs, Florida 32701 - Phone: (407) 960-1717
- Fax: (407) 834-2500
Davenport
- Address: 2310 North Blvd, Davenport, FL 33837
- Phone: (407) 960-1717
- Fax: (407) 834-2500
Delray
- Address: 15300 Jog Rd,
Suite # 107-108
Delray Beach, FL 33446 - Phone: (561) 630-1611
- Fax: (561) 630-1613
Fort Pierce
- Address: 2401 Frist Blvd.
Suite # 7
Fort Pierce, FL 34950 - Phone: (772) 466-0088
- Fax: (772) 460-8555
Hollywood
- Address: 3500 Tyler Street Hollywood, Florida 33021
- Phone: (954) 987-2047
- Fax: (954) 987-2048
Miami
- Address: 11401 SW 40th St.
Suite # 120
Miami, FL 33165 - Phone: (954) 987-2047
- Fax: (954) 987-2048
Orlando
- Address: 6150 Metrowest Blvd.
Suite #102
Orlando, Florida 32835 - Phone: (407) 960-1717
- Fax: (407) 834-2500
Palm Beach Gardens
- Address: 3355 Burns Road . Suite 304, PBG, Florida 33410
- Phone: (561) 630-1611
- Fax: (561) 630-1613

